Table of Content
- What does your liver do?
- What is the most common liver disease?
- What are Liver Function Tests?
- What about other liver diseases?
- What are pathologists looking for when they examine a liver biopsy?
- Do I need Liver Function Tests (LFTs)?
If you feel well, don’t drink alcohol, eat a healthy diet, exercise regularly and don’t have any additional risk factors such as Haemochromatosis, diabetes, obesity, high blood pressure or high cholesterol then your liver is probably in reasonably good shape.
However, a recent study revealed that deaths from Non-alcoholic Fatty Liver Disease (NAFLD) are set to rise 90% by 2030, so taking part in Dry July is not the only factor in protecting your liver health.
Richard Wylie, CEO of the Liver Foundation said; “The key to winning against liver disease is action. Go and see your doctor. Learn about your disease. Make sure you follow the advice that has been given. And finally, keep following up and participate in whatever screening and testing has been recommended”.
According to the Liver Foundation, liver cancer is the fastest growing cause of cancer deaths in Australia. We asked some pathologists about liver health and what pathology tests can tell us.
What does your liver do?
The liver is the largest internal organ and is very important for survival and overall health. On its way around the body, your blood will go to the liver to be detoxified of any harmful substances such as drugs. The liver also produces bile which is used for digestion in the intestines and stored in the gall bladder.
What is the most common liver disease?
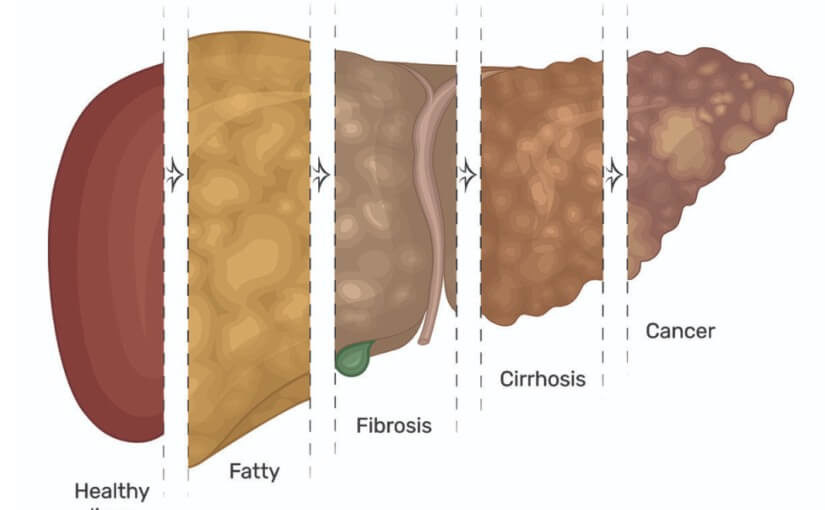
One of the most common liver problems is fatty liver disease. This is a group of diseases that affects 20-30% of the population and in the early stages usually doesn’t have symptoms.
Fatty liver disease occurs when the liver is not breaking down fats as it normally should and so fat builds up in the liver. The condition has been linked to other health problems such as diabetes, obesity or metabolic syndrome, but it can affect people who don’t have these risk factors.
Fatty liver disease can also be caused by excessive alcohol consumption and the condition is divided into alcoholic fatty liver disease or non-alcoholic fatty liver disease (NAFLD). The non-alcohol related condition is more common and is said to be on the rise in many countries, including Australia, which may be partly due to higher consumption of foods with added sugar and fat. In reality, in Australia, because alcohol consumption and obesity are common, many people will have contributions from both in their fatty liver disease.
Fatty liver disease can cause the liver to become inflamed (known as steatohepatitis) and over time this can cause scarring of the liver known as cirrhosis. Liver cirrhosis is serious, it can cause liver failure and can lead to cancer. That is why diagnosing fatty liver disease early is important to prevent damage to the liver and mitigate the risk of more serious disease in future.
What are Liver Function Tests?
Liver Function Tests (LFTs) are a group of tests looking at various substances in the blood that give clues about the health of the liver. LFTs measure enzymes, proteins, and substances that are produced or excreted by the liver and are affected by liver injury.
LFT abnormalities are not only early indicators of a liver condition, but patterns of test abnormalities may also indicate the type of disease process involved.
Chemical pathologist Dr Que Lam says LFT results must be carefully interpreted;
“Aside from fatty liver, we frequently see viral liver disease (hepatitis) and toxic damage from prescribed and non-prescribed drugs and alcohol.
Liver function tests reflect the current state of the liver. Not all conditions are permanent and test results may return to normal in some situations. For example, LFT changes may be brought about by short term antibiotic use, and return to normal when the antibiotics are ceased. Often, to confirm a continuing disease process, LFTs need to be repeated after a few days or weeks to determine whether the test abnormalities have resolved, persist or have progressed.”
What about other liver diseases?
Although LFT results may give your doctor enough information to treat you, in some cases they may also recommend a liver biopsy.
Many liver conditions can be diagnosed through a liver biopsy and a biopsy is most commonly ordered when LFTs from the chemical pathology area have come back with abnormalities, or imaging such as an MRI scan has shown a mass or lesion in the liver.
The most common way a biopsy can be taken is through the skin with a needle, often using an ultrasound scan to help guide the needle, and in pathology the sample is referred to as a ‘core’. A liver core is a small piece of tissue usually between 10-20mm in length and just 1.2mm wide but it can give the pathologist a lot of information about the health of the patient’s liver.
A liver biopsy is examined in the laboratory by an anatomical pathologist, using a microscope.
A liver biopsy may also be needed to investigate the cause of jaundice. This is when the skin and/or whites of the eyes have a yellow appearance due to an increased level of bilirubin in the blood. Bilirubin is usually processed in the liver so jaundice can be a sign of a problem in the liver.
What are pathologists looking for when they examine a liver biopsy?
Anatomical Pathologist, Dr Julie Lokan explains; “What we look for depends in part on the type of sample and the clinical notes and patient history we are given by the referring doctor. In the case of jaundice we would look for an explanation of liver dysfunction such as a blocked bile duct that could cause bilirubin to build up in the blood. As liver cell dysfunction due to various causes (such as viral hepatitis or drug induced liver injury) can also cause jaundice, then we might consider those possibilities in the differential diagnosis.
If the sample has come from a lesion, then we will determine if it is benign or malignant, or if it’s something else that’s mimicking a tumour.
We look for a recognisable pattern and we discuss what we have found with our clinical colleagues then put the data together with results from any imaging a patient might have had to reach a diagnosis.”
Liver biopsies may also be needed to determine the level of chronic damage done to the liver by a disease such as hepatitis or fatty liver disease.
Although there is now a vaccine for Hepatitis B there are still cases in some communities in Australia, so it is still important to get a diagnosis (or rule it out) if factors indicate a person is at risk. Hepatitis C can now be cured with the latest drugs so diagnosis is very important to ensure the best treatment.
Do I need Liver Function Tests (LFTs)?
If you have concerns about your liver health, talk to your doctor. They can assess what tests (such as LFTs) you may need, and also talk to you about lifestyle, medication or anything else you are worried about with regards to liver health.
Associate Professor Simone Strasser is President of the Gastroenterological Society of Australia, she said;
“Your GP is the best person to assess whether you might have a problem with your liver. They will do an initial assessment, but if there are any concerns about the diagnosis or that liver injury is putting you at risk, they may refer you to a liver specialist. A liver specialist will recommend any specific treatments for liver disease and monitor for complications. By being proactive and ensuring your liver condition is diagnosed, treated and monitored, the chance of dying from liver cancer or liver failure is significantly reduced”.
If you have any symptoms that concern you, it is essential not to delay getting medical help. Like many chronic conditions NAFLD usually has no symptoms early on. Even vague symptoms such as unusual fatigue could point towards an issue, and if it’s not your liver causing the problem, it’s always worth ruling out a liver issue and finding out the true cause. Fortunately, pathology has the answers your doctor needs to know, so get along to your GP if you’re not feeling 100%.
References:
*image credit: Getty via https://medicine.wustl.edu/news/study-reveals-links-between-fatty-liver-disease-liver-cancer/